
Sleep Hygiene
December 22, 2020 in Educate Yourself, LINKS
 The amount of sleep I’ve had in any given night is the single most important determinant in how my day is going to go. This is because sleep correlates with emotional well-being, physical health and ability to concentrate and function properly throughout the day. I find myself especially cranky and kind of insufferable to be around on days that I haven’t had enough sleep – I’m one of those “don’t talk to me until I’ve had coffee” kind of people.
The amount of sleep I’ve had in any given night is the single most important determinant in how my day is going to go. This is because sleep correlates with emotional well-being, physical health and ability to concentrate and function properly throughout the day. I find myself especially cranky and kind of insufferable to be around on days that I haven’t had enough sleep – I’m one of those “don’t talk to me until I’ve had coffee” kind of people.
There’s a ton of science backing up the connection between good sleep and general well-being, in literally every single aspect of our lives. The book Why We Sleep by Matthew Walker gives a comprehensive background of sleep research, in non-scientific language that makes it really interesting and easy to read, so I’d highly recommend it to anyone looking to learn more about how to better their sleep. For example, the book states, “Within the brain, sleep enriches our ability to learn, memorize, and make logical decisions. It recalibrates our emotions, restocks our immune system, fine-tunes our metabolism, and regulates our appetite.”
Sleep hygiene is made up of both creating an environment that is conducive to your individual sleep needs and forming good habits that allow your body and mind to get the good sleep that it needs.
 Have set sleep times
Have set sleep times
Especially for those struggling with sleep in relation to mood disorders such as depression and anxiety, psychologists recommend having the same wake up time each day, as well as the same sleep time each day. This is so your body becomes used to a sleep routine and is able to fall asleep more easily.
Your bed is for sleeping
It’s important to create a mental connection between sleeping and being in your bed, so it’s recommended to avoid lounging in bed and working in bed during the day. This is especially harder now that we’re all working from home, especially if your desk is in your bedroom, but still important!
Don’t toss and turn
If you’ve been in bed trying to sleep unsuccessfully for 30 mins, get up and stretch or have a glass of water and read for a few minutes before getting back into bed to try again. I find this helpful as I tend to get more and more frustrated with myself if I can’t sleep, and that makes it even harder because then I’ve worked myself up!
What is your sleep like? How do you think your sleep habits currently affect your mood? Have you ever changed your habits, and if so, what did you do?












 For most people, social media is an intrinsically large part of our lives. Young people can easily spend hours per day on various social media networks without even realizing they are doing so. Enabling phone notifications for these apps means that we log onto these networks multiple times a day to see the newest updates and posts, including comments and likes on our own posts.
For most people, social media is an intrinsically large part of our lives. Young people can easily spend hours per day on various social media networks without even realizing they are doing so. Enabling phone notifications for these apps means that we log onto these networks multiple times a day to see the newest updates and posts, including comments and likes on our own posts.
 Get a referral If you are a college student, most university wellness/counseling centers will do a quick 15 minute screening for free. This means that you’ll speak with somebody briefly, explaining what you are seeking services for, and they’ll give you a long list of therapists in the area that they recommend. If you are not in college, PCP offices will also do this for you!
Get a referral If you are a college student, most university wellness/counseling centers will do a quick 15 minute screening for free. This means that you’ll speak with somebody briefly, explaining what you are seeking services for, and they’ll give you a long list of therapists in the area that they recommend. If you are not in college, PCP offices will also do this for you!
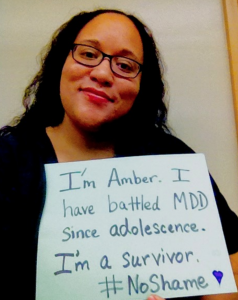
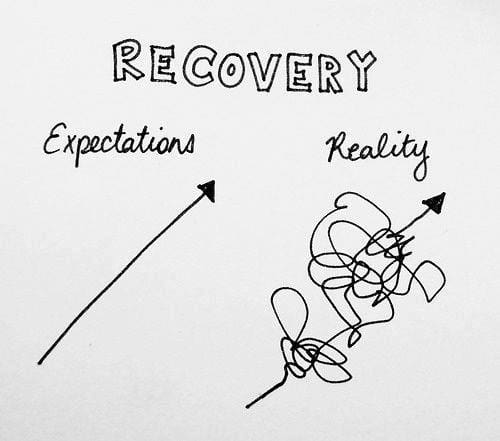 Recovery from mental illness is not always a straight line in an upward trajectory. In fact, the path to recovery is almost never straight and easy. There isn’t necessarily even a discernible end goal—a point that you’ll reach when you can say, “I’m done recovering.”
Recovery from mental illness is not always a straight line in an upward trajectory. In fact, the path to recovery is almost never straight and easy. There isn’t necessarily even a discernible end goal—a point that you’ll reach when you can say, “I’m done recovering.”
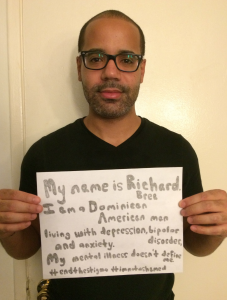
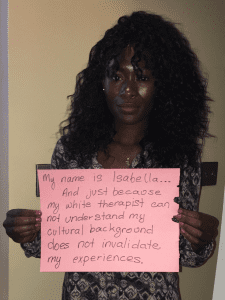 Mental illness is often seen as a “white person’s disease”—a product of privilege, a chosen illness. It is represented in the media by people who are white, while those who are not suffer in silence. The most important thing to remember is that mental illness does not discriminate according to race—or any other demographic, including class, gender, and so on.
Mental illness is often seen as a “white person’s disease”—a product of privilege, a chosen illness. It is represented in the media by people who are white, while those who are not suffer in silence. The most important thing to remember is that mental illness does not discriminate according to race—or any other demographic, including class, gender, and so on.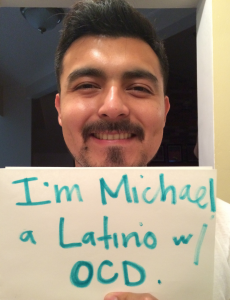
Recent Comments